To the Editor of The Keene Sentinel:
Please run an error correction for your Sept. 10-11 front-page headline:
“As the pandemic subsides, college presidents course correct”
And the electronic and filename versions are even worse:
“As pandemic ends, college presidents course correct”
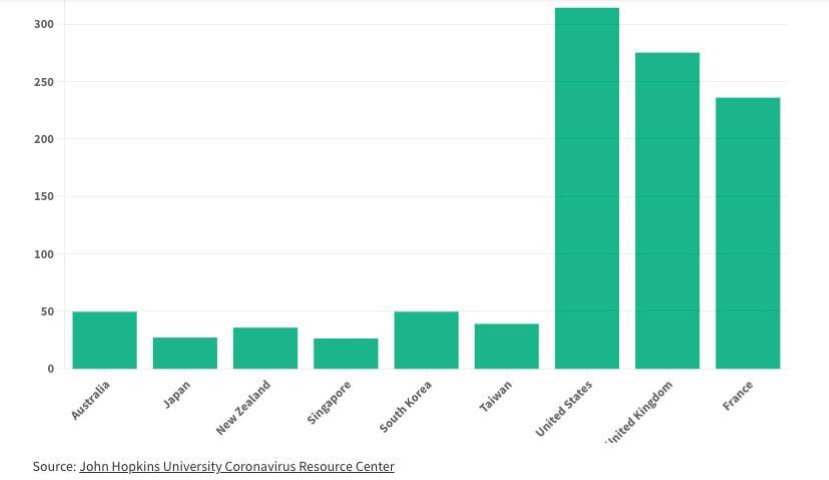
No responsible party is saying the pandemic is over—or even “subsiding". Just the opposite. For example, the same weekend, the Wall Street Journal ran a story: "Covid-19 Is Still Killing Hundreds of Americans Daily”. Over the past few months, the more-or-less 400 daily deaths translate to about 150,000 a year at this rate. (This is three times the highest annual flu deaths in the past decade.) In New Hampshire, our rate of community spread and deaths this summer is about twice that of last year.
And the fall surge hasn’t even started yet. The Biden administration has warned that the U.S. could see 100 million COVID-19 infections in the fall and winter. As students go back to school, and people of all ages go inside buildings with less fresh air, and the virus remains active with more variants in the pipeline, a fall/winter surge seems inevitable. Take a look at the graph below of NH deaths, courtesy of Covid Act Now.
As an engineer who has been dealing with the pandemic since the first summer, I know that there are many simple actions that people and building managers can take to reduce the spread and risk. They include increased fresh air ventilation, antigen tests by the right people at the right time, and highly effective masks for higher-risk situations. (These and other topics, including fresh air meters and other tools, are presented on my website at https://www.kohlerandlewis.com/covid-19blog .)
Instead of declaring the pandemic to be ending, it would be more useful if The Sentinel would run a weekly reminder as long as it is still here, such as a graph of the average daily covid-19 deaths over the last 6-12 months.
Roy Swain
Westmoreland
Now You Can Search This Blog!
We have added a “search” bar for this blog - scroll all the way down
to the very bottom of a blog page to find the search bar.
We invite you to subscribe to our Newsletter -
the cost is free and each new post comes to your email
every two weeks on Thursdays!
To subscribe, simply email safetulator@kohlerandlewis.com
with your name and email address and we will sign you up.
Highlights From Past Blogs
June 30 - Summer Gatherings Can Be Safer
June 22 - Summer Gatherings Can Be Safer
May 31 - Covid Myth-Busting
April 29 - The Big Meter
April 19 - The Spring Surge Is Here
April 7 - How to Test
March 21 - The Origin of the CDC’s Biggest Mistake
February 25 - One. Million. Deaths.
February 16 - Ventilation Revolution
January 11 - Air Purifiers
January 4 - Masks That Actually Work
December 15 - The Double Risk of Indoor Dining